
By D. Kenton Henry
Editor, Agent, Broker
Finding Your Doctor and Understanding Subsidies in HMO Plans
Shopping for individual or family health insurance can feel like navigating a maze—with dead ends, confusing signs, and few clear answers. Two of the most common pain points for shoppers are (1) trying to keep your current doctor while limited to an HMO network and (2) figuring out whether you qualify for a subsidy, known as an advance premium tax credit (APTC). Both challenges can make the process frustrating and overwhelming, especially during open enrollment when time is limited.
The HMO Headache: “Will My Doctor Be Covered?”
One of the biggest shocks people face when shopping for health insurance is realizing that their trusted doctor or medical provider might not be covered under a new plan—especially if it’s an HMO (Health Maintenance Organization). Unlike PPOs (Preferred Provider Organizations), which offer broader provider access and out-of-network options, HMO plans restrict coverage to a specific network of doctors and hospitals. If your doctor isn’t in the network, you may have to pay the full cost of your visit out of pocket—or switch doctors entirely.
Unfortunately, trying to find this information is often easier said than done.
- Outdated or Inaccurate Provider Directories: Online directories can be incomplete or outdated. It’s not uncommon for a provider to be listed as “in-network” only for you to find out later they’ve left the plan.
- Hard-to-Navigate Insurance Websites: Many insurance carrier sites don’t make it easy to search by doctor name, location, or specialty. Even worse, each plan may have its own “network tier,” adding another layer of complexity.
- No Universal Search: There’s no centralized tool that lets you enter your doctor’s name and see every marketplace plan that includes them. You have to check each insurance company or plan individually.
For people with ongoing care needs—like managing chronic conditions or continuing with a trusted pediatrician or specialist—the possibility of switching providers isn’t just inconvenient, it can feel risky.
The Subsidy Puzzle: “Do I Qualify for Help Paying My Premium?”
The Affordable Care Act (ACA) made health insurance more accessible by offering subsidies for people who meet certain income guidelines. These subsidies, officially called advance premium tax credits, lower your monthly premium based on your household size and income.
The good news is that many people qualify.
The bad news is that determining whether you qualify can feel like filling out a tax return just to get a quote.
- Income Guesswork: Subsidy eligibility is based on your estimated household income for the upcoming year. That’s right—you must predict your future income, even if you’re self-employed or work variable hours.
- Family Dynamics Matter: Your household size includes dependents—even if they don’t need insurance—and income from every working member. This means getting it right often requires gathering data from multiple people.
- Mid-Year Changes Complicate Things: If your income or family size changes mid-year, you may need to report it or risk having to repay part of your subsidy at tax time.
- The ACA “Cliff” and “Glide Path”: Previously, you could lose your subsidy entirely if your income was even $1 over the limit. Recent changes have smoothed this out, but they are still complicated and frequently misunderstood.
And while tools like Healthcare.gov’s calculator are helpful, they often rely on broad estimates. They can’t account for all variables, such as gig work, investment income, or multiple part-time jobs.
Why It Feels So Frustrating
When you shop for health insurance, you’re not just picking a product—you’re making decisions that affect your finances, your family’s well-being, and your access to care. The stakes are high, yet the process often feels opaque and unnecessarily complicated.
You’re expected to:
- Compare dozens of plans with unfamiliar terms,
- Check if your providers are covered (without reliable tools),
- Predict your income a year in advance,
- And hope you don’t make a mistake that costs you money or coverage.
Tips for a Smoother Experience
While the system isn’t perfect, there are ways to reduce frustration:
- Use a Licensed Agent or Broker: Agents specializing in ACA plans can often help you find plans that include your provider and determine if you qualify for subsidies—all at no extra cost.
- Call Your Doctor’s Office: Don’t rely solely on insurance directories. Call your provider’s office directly to confirm if they accept a specific plan.
- Keep Documentation: If your income fluctuates, keep clear records. This will help you provide accurate estimates and support your case in the event of an audit or dispute.
- Update Changes Promptly: If your income or household size changes mid-year, report it on your health insurance marketplace to avoid surprise bills or tax penalties.
In Summary
Shopping for individual or family health insurance can be a stressful process—especially when you’re trying to keep your doctor and figure out if you qualify for financial help. Between restrictive HMO networks and confusing subsidy rules, it’s easy to feel stuck. But with a little extra diligence, some expert help, and the right questions, you can find a plan that fits your needs without sacrificing peace of mind.
If the process still feels overwhelming, you’re not alone. Many Americans share the same frustrations—and continue to hope for a more user-friendly system in the future.
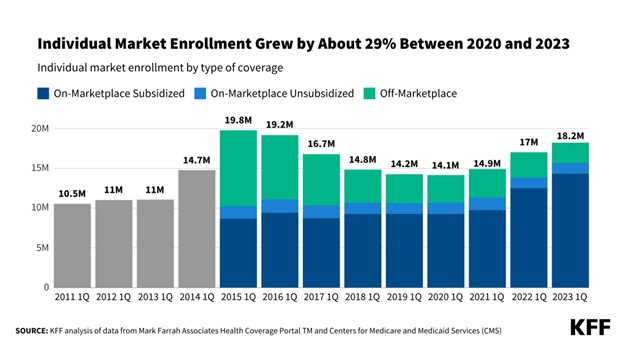
Below is a chart outlining estimated income thresholds for qualifying for an Advance Premium Tax Credit (APTC) in 2025. These thresholds are based on a percentage of the Federal Poverty Level (FPL), which is adjusted annually. For simplicity, the chart includes 2024 FPL figures (used for 2025 coverage) and the income ranges (100%–400%+ of FPL) where most people qualify for subsidies under the ACA.
📝 Note: Due to the American Rescue Plan and Inflation Reduction Act, subsidies may extend beyond 400% of the FPL, with a sliding scale that caps the percentage of income spent on premiums. These extended subsidies are currently in place through 2025.
2024 Federal Poverty Level (FPL) and APTC Income Guidelines for 2025 Coverage
Household Size100% / FPL400% / FPLTypical APTC Eligibility Range
1 (Individual) $14,580 / $58,320 / $14,580 – ~$58,000+
2 (Couple) $19,720 / $78,880 / $19,720 – ~$79,000+
3 $24,860 / $99,440 / $24,860 – ~$99,000+
4 (Family) $30,000 / $120,000 / $30,000 – ~$120,000+
5 $35,140 / $140,560 / $35,140 – ~$141,000+
6 $40,280 / $161,120 / $40,280 – ~$161,000+
Key Notes:
- Minimum Income: You must earn at least 100% of the FPL to qualify for a subsidy in most states. In Medicaid expansion states, if you earn less than 138% FPL, you may qualify for Medicaid instead.
- Upper Limit Removed: Thanks to temporary reforms, people earning above 400% FPL may still qualify for a subsidy if the cost of the benchmark plan exceeds ~8.5% of their income.
- Household Size: Includes you, your spouse, and any dependents claimed on your tax return.
💡 What This Means for You
- If your estimated annual income falls between the ranges shown above, you likely qualify for help paying your monthly health insurance premium.
- Households earning more than 400% of the FPL may still qualify if their premiums exceed about 8.5% of income, thanks to current federal subsidy expansions.
- Eligibility is based on your tax household — including you, your spouse, and dependents you claim on your tax return.
- If your income is below 138% FPL, you may qualify for Medicaid (in most states).
DO NOT CALL AN 800 NUMBER and talk to some anonymous employee of an insurance company. Not only are they restricted to limiting you exclusively to their company’s options—but your personal information will be instantly sold and shared. Your phone is going to begin ringing off the hook!
I’ve been specializing in Medicare-related insurance for over thirty years, right here in The Woodlands, Texas, USA! I represent every Medicare-related product, including Supplement, Advantage, and Part D Drug plans, from virtually every “A” rated company doing Medicare-related business in Texas. And I CHARGE NO FEE for my services! Deal with a local agent/broker who values your business enough not to share it with anyone!
D. Kenton Henry
Editor, Agent, Broker
Office: 281.367.6565
Text my cell 24/7 @713.907.7984
Email: Allplanhealthinsurance.com@gmail.com

https://www.woodlandsonline.com/blps/article.cfm?page=14062
Https://TheWoodlandsTXHealthInsurance.com
Https://Allplanhealthinsurance.com
https://healthandmedicareinsurance.com/2025/03/20/congratulations-youre-turning-age-65-and-eligible-for-medicare-whats-next/?fbclid=IwY2xjawJKSbBleHRuA2FlbQIxMQABHQbe0u7yebhaHWAa_6axQnzaMdTi9mM6TUvKICB6PZT-xV45uXovIMtEog_aem_0lPN3F7TsqV6X7pjJLvLJg






Leave a comment